
Contents:
Non-insulin anti-diabetic medications
Mechanism of action:
Reduce insulin resistance
Reduce hepatic glucose output
Increase peripheral glucose utilisation
Increase glucose turnover between intestine and liver
Main elimination route: Renal
Precautions:
- GI intolerance
- Lactic acidosis (rare)
- Renal impairment
- Hypoglycaemic condition
Name: Metformin
Starting dose: 500mg BD
Max dose: 1g BD
Mechanism of action:
Directly increase insulin secretion
Binds to SUR1 – stimulates β-cells by closure of K+-ATP channels
Main elimination route: Renal 60%
Precautions:
- Hypoglycaemia
- Selection restricted by severe liver or renal disease, or porphyria
Name: Gliclazide
Starting dose: 40mg OD
Max dose: 320mg/24hrs
Name: Gliclazide SR
Starting dose: 30mg OD
Max dose: 120mg OD
Mechanism of action:
Directly increase insulin secretion
Binds to benzamido site on SUR1 – stimulates βcells by closure of K+- ATP channels
Rapid onset, short duration of action
Main elimination route: Hepatic
Precautions:
- Lesser risk of hypoglycaemia (fewer and less severe than with sulphonylureas)
- Liver or severe renal disease
Names: Nateglinide
Starting dose: 60 mg with each meal
Max dose: 540mg
Names: Repaglinide
Starting dose: 0.5g with meals
Max dose: 16g
Mechanism of action:
Increase insulin secretion
Inhibition of DPP-4 allows increased t½ for incretins, which potentiate nutrientinduced insulin secretion
Main elimination route: Sitagliptin – Renal, Linagliptin – Faecally excreted
Precautions:
- Small risk of hypoglycaemia (seldom severe), mostly when used with other glucose lowering agents
- Substantial renal or liver disease
Names: Sitagliptin
Starting dose: 50mg OD
Max dose: 100mg OD
Names: Linagliptin
Starting dose: 5mg OD
Max dose: 5mg OD
Mechanism of action:
Increase insulin action
Stimulate PPARγ increase adipogenesis
Alter glucose-fatty acid cycle
Main elimination route: Hepatic
Precautions:
- Heart failure, oedema, fluid retention
- Anaemia
- Fractures
- Cardiac disease
- Severe liver or renal disease
Names: Pioglitazone
Starting dose: 30mg OD
Max dose: 45mg OD
Mechanism of action:
Inhibiting the digestion of carbohydrates by inhibiting a-glucosidase
Main elimination route: Renal 35%
Precautions: The major drawback of acarbose is the fact that it is often associated with a lot of flatulence.
Names: Acarbose
Starting dose: 50mg OD
Max dose: 100mg TDS
Mechanism of action:
Reversibly inhibits SGLT2 to reduce glucose reabsorption and increase urinary glucose excretion
Main elimination route: Hepatic and Renal
Precautions:
- Risk of DKA, use with caution conditions leading to restricted food intake.
- Renal impairment.
Names: Canagliflozin
Starting dose: 100mg OD
Max dose: 300mg OD
Names: Dapagliflozin
Starting dose: 10mg OD
Max dose: 10mg OD
Names: Empagliflozin
Starting dose: 10mg OD
Max dose: 25mg OD
Mechanism of action:
Increase glucose dependent insulin secretion
Reduce gastric emptying
Main elimination route: Renal
Precautions:
- CCF
- Pancreatitis
- Renal impairment
Names: Albiglutide
Starting dose: 30mg weekly
Max dose: 50mg weekly
Names: Exenatide
Starting dose: 5mcg BD
Max dose: 10mcg BD
Names: Liraglutide
Starting dose: 0.6mg OD
Max dose: 3mg OD
Names: Lixisenatide
Starting dose: 10mcg
Max dose: 20mcg
Types of Insulin
Novorapid
- Source: Analogue
- Delivery system: Vial and syringe, or 3ml cartridges in a re-usable pen, or pre-filled disposable pen system (Flexpen)
- Taken: Just before / with / just after food
- Time action profile:
- Rapid-acting insulin analogue

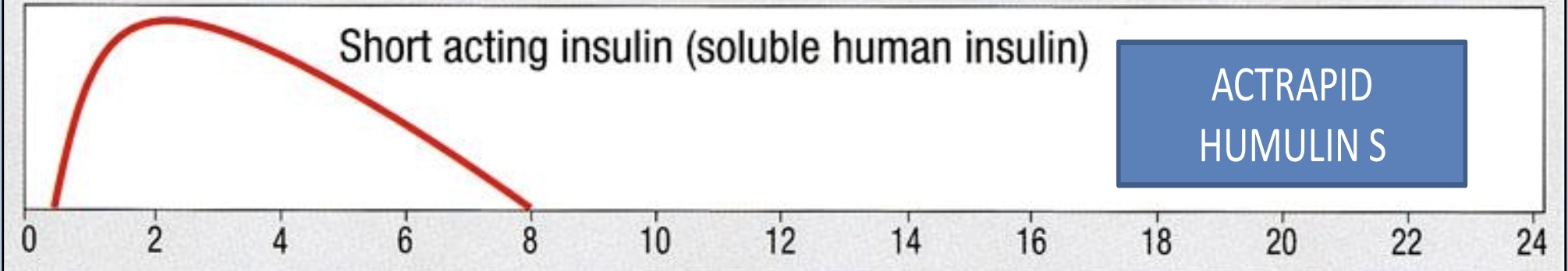
Actrapid
- Source: Human
- Delivery system: Vial and syringe
- Taken: For use only in VRIII or FRIII
- Time action profile:
- Short-acting insulin (soluble human insulin)
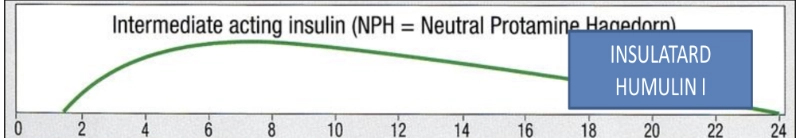
Humulin
- Source: Human
- Delivery system: Vial and syringe, or 3ml cartridges in a re-usable pen, or pre-filled disposable pen system (Kwikpen)
- Taken: 30 mins before food
- Time action profile:
- Intermediate-acting insulin (NPH = Neutral Protamine Hagedorn)
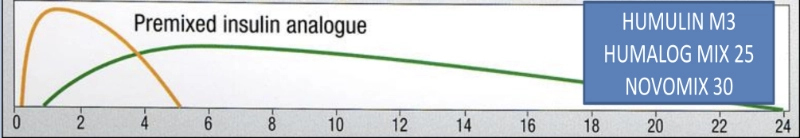
Humalog Mix25
- Source: Analogue
- Delivery system: 3ml cartridges in a re-usable pen, or pre-filled disposable pen system (Kwikpen)
- Taken: Just before / with / just after food
- Time action profile:
- Premixed insulin analogue
NovoMix 30
- Source: Analogue
- Delivery system: 3ml cartridges in a re-usable pen, or pre-filled disposable pen system (Flexpen)
- Taken: Just before / with / just after food
- Time action profile:
- Premixed insulin analogue
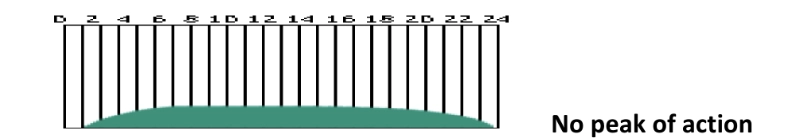
Lantus
- Source: Analogue
- Delivery system: Vial and syringe, or 3ml cartridges in a re-usable pen, or pre-filled disposable pen system (Solostar)
- Taken: Once a day anytime but at the same time each day
- Time action profile:
- No peak of action
Levemir
- Source: Analogue
- Delivery system: Vial and syringe, or 3ml cartridges in a re-usable pen, or pre-filled disposable pen system (Solostar)
- Taken: Once a day anytime but at the same time each day
- Time action profile:
- No peak of action
Simplifying an insulin regime
Simplifying an insulin regime by converting from a twice daily mixed insulin to once daily long-acting insulin is done by understanding the proportion of intermediate-acting insulin in it. For example Novomix 30 has 70% intermediate-acting insulin. Humalog 25 has 75% intermediate acting insulin. Calculate the total daily amount of intermediate-acting insulin and give 80% of this amount as LA insulin analogue such as Lantus once daily. If blood glucose is low i.e. 4.0- 6.0 mmol/L, use 50% of the original intermediate-acting dose.
For example
If the patient normally takes 20 units BD Novomix 30, this totals 40 units of insulin in 24 hours as it is a BD preparation. This is a mixture of intermediate and short acting insulin.
70% of Novomix 30 is intermediate-acting, so the patient takes 28 units of intermediate-acting insulin daily (0.70 x 40 units = 28 units).
To calculate the new dose, we want 80% of the existing intermediate-acting daily insulin dose, which is 22 units (0.80 x 28 units = 22 units).
If hypoglycaemic we need to give 50% of the daily intermediate-acting insulin dose. This equals 14 units (0.50 x 28 units = 14 units)
Disclaimer
These Guidelines are intended for use by healthcare professionals and the expectation is that they will use clinical judgement, medical, and nursing knowledge in applying the general principles and recommendations contained within. They are not meant to replace the many available texts on the subject of palliative care.
Some of the management strategies describe the use of drugs outside their licensed indications. They are, however, established and accepted good practice. Please refer to the current BNF for further guidance.
Whilst SPAGG takes every care to compile accurate information , we cannot guarantee its correctness and completeness, and it is subject to change. We do not accept responsibility for any loss, damage or expense resulting from the use of this information.
