
Contents:
In event of a catastrophic bleed:
It is important to remember, that in the event of a massive, terminal bleed the patient may be unconscious within minutes and may die very quickly, even before the sedation has had a chance to work. Thus, it is important to remember that whilst sedation is important, never leave the patient alone, and always stay with them.
- Stay calm and if possible, summon assistance.
- Ensure that someone is with the patient.
- If possible, nurse in recovery position to keep airway clear.
- Stem / disguise bleeding with dark towels.
- Apply pressure to the area if bleeding from external wound with haemostatic dressings/gauze or adrenaline soaks if available.
- Administer crisis medication if prescribed which can be repeated after 10 minutes if needed.
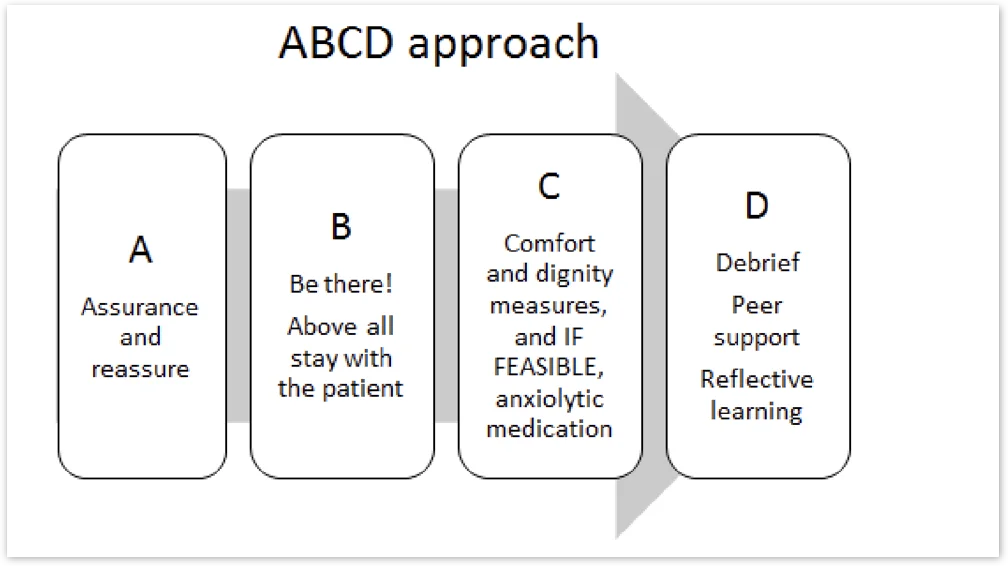
- Events of this nature are likely to be distressing to relatives/carers and staff. Offer support, opportunity to debrief, follow up with chaplaincy and psychological support to everyone involved.
Drug
MIDAZOLAM
Route* & Onset of effect
Intramuscular preferably deltoid 5–15 minutes
Dose **
10 mg
Frequency
Repeat after 10 minutes if needed
* The subcutaneous route is inappropriate due to peripheral shut down and unpredictable absorption.
* If the patient is already on large background doses of midazolam or other benzodiazepines, but still not adequately sedated during catastrophic bleeding they may need larger doses of midazolam in proportion with the background dose.
In summary:
Non-Terminal Bleed:
In the event that a major bleed does not rapidly result in death, urgent assessment and plans for ongoing care / treatment need to be made.
Treatment and care plans will depend on the patient’s clinical condition, expected prognosis, likely source/site of bleeding, and wishes and preferences.
For those with persistent major bleeding and expected to die soon, consider an infusion of midazolam to manage ongoing anxiety or distress.
If bleeding appears to have stopped or reduced, a full assessment is required to ensure the risk of further distressing bleeding is minimised appropriately. Haemostatic gauze/granules, if used, can be left in situ for up to 24 hours before being gently removed.
Disclaimer
These Guidelines are intended for use by healthcare professionals and the expectation is that they will use clinical judgement, medical, and nursing knowledge in applying the general principles and recommendations contained within. They are not meant to replace the many available texts on the subject of palliative care.
Some of the management strategies describe the use of drugs outside their licensed indications. They are, however, established and accepted good practice. Please refer to the current BNF for further guidance.
Whilst SPAGG takes every care to compile accurate information , we cannot guarantee its correctness and completeness, and it is subject to change. We do not accept responsibility for any loss, damage or expense resulting from the use of this information.
